Cloud computing is the delivery of your computing needs as a service rather than as a suite of products that you have to purchase and maintain. Why couldn’t we do that with an EMR or EHR for our patients?


Cloud computing is the delivery of your computing needs as a service rather than as a suite of products that you have to purchase and maintain. Why couldn’t we do that with an EMR or EHR for our patients?

As the physicians of the baby boomer generation approach their golden years, many have achieved career and financial success and are looking for an arrangement that will allow them to ease into retirement. While you may not be ready to hang up your white coat permanently, you may be interested in working fewer hours and taking less call. Retirement requires more than simply removing your name from the office door, however. If you are a physician nearing retirement, it is important that you plan, discuss and make contractual agreements that will allow you to accomplish your goals and changing needs.
The Patient Protection and Affordable Care Act of 2010 (ACA) is described as the most sweeping health care legislation passed in the U.S. since Medicare’s implementation in 1965. The health reform law is already changing the health care system, but the most profound modifications are yet to come. The law will affect otolaryngologists’ practices in many ways, both direct and indirect. Here are some areas of the law to consider.

October 1, 2013 should be on the mind of every physician in the U.S. That is the day when a new diagnostic coding system will be instituted, the first such change since 2003. The implementation’s aftermath is predicted to be anywhere from a normal day at the office to financial Armageddon.
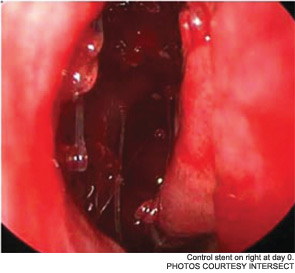
Maintaining sinus patency after functional endoscopic sinus surgery (FESS) for chronic rhinosinusitis (CRS) has long been an issue; as many as 23 to 47 percent of patients require revision surgery after FESS. Now, a new drug-eluting, bioabsorbable stent manufactured by Intersect (Palo Alto, Calif.) is being billed as a “breakthrough treatment [that] improves outcomes for sinus surgery,” according to a news release from the company. The device, which received pre-market approval from the U.S. Food and Drug Administration (FDA) in August, has been studied since 2008. It is currently available in Texas, New York, Philadelphia, New Jersey, Atlanta, Ohio and Kentucky.
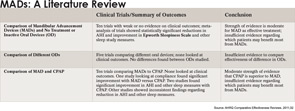
Oral appliances may work better than CPAP for some patients

Every otolaryngology group needs a chance to evaluate its organization outside the frenetic pace of day-to-day patient care. A practice retreat provides the opportunity to assess your operations, examine your mission and conduct strategic planning in a setting where physicians are relaxed and undistracted.

What’s more important, your computer’s hardware or its software? You tell me: What’s more important, your heart or your lungs? Obviously, if you’re going to function, you need both. The same is true for electronic medical record (EMR) and electronic health record (EHR) software: Your hardware is mission-critical to the success of your electronic records, and this is not the place to compromise.

Residents in the general surgery program at Washington University in St. Louis, Mo., participate in monthly “pizza grand rounds,” in which they discuss ethics-fraught situations they encounter. Some of the situations are the subjects of papers published in Surgery. Here are summaries of a few of those published situations. The papers intentionally do not mention the actions ultimately taken, so that the attention remains on the principles and questions involved.

Have you ever wondered about the reasoning behind hospital discharge paperwork or the requirement that every patient sign a HIPAA form?Here are explanations for some of the health care policies you come across on a daily basis.